Rhode Island ranks fourth in the nation in the Commonwealth Fund’s 2025 State Health System Scorecard, reflecting years of progress in access, quality, and equity. This is an achievement to celebrate—but behind that strength lies a growing affordability challenge for employers and families.
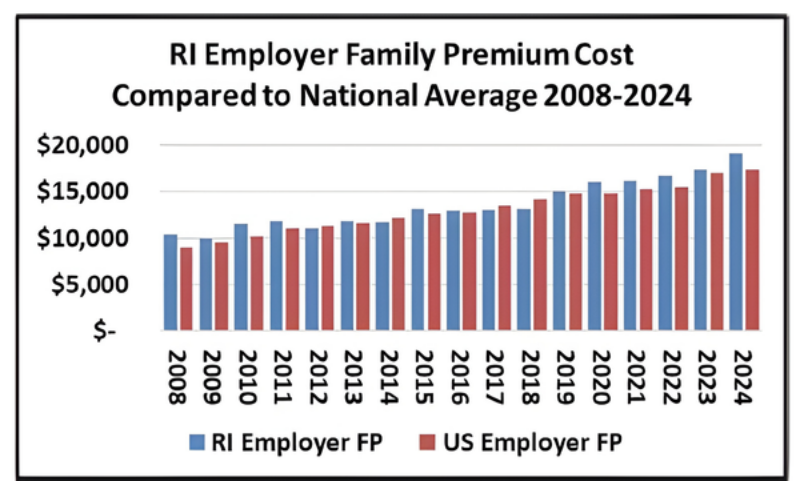
The Commonwealth Fund’s affordability metric draws in part from the Medical Expenditure Panel Survey – Insurance Component (MEPS-IC), which measures premiums and employer contributions for job-based coverage. Because employers pay most of the cost of family plans, the Rhode Island Business Group on Health (RIBGH) analyzed the same data to assess affordability from the employer’s perspective.
Between 2019 and 2024, Rhode Island’s average family premium rose from 102% to 110% of the national average. For most of the 2008–2024 period, Rhode Island tracked close to the
national average, but in recent years costs have accelerated, widening the gap. With approved 2026 commercial premium increases exceeding 20%, Rhode Island’s employer costs will move still further above the U.S. average.
These higher premiums have real economic consequences—reducing business competitiveness, limiting wage growth, and straining household budgets. They also risk weakening the state’s overall economic vitality.
Rhode Island’s strong performance on access, quality, and equity remains an asset, but long-term sustainability depends on addressing rising hospital and system costs. RIBGH will continue monitoring employer-sponsored premiums and advocating for evidence-based hospital payment reform, cost transparency, and accountability—to ensure that Rhode Island’s health system remains not only high-performing but also affordable for employers and families alike.
